The Common Vein Copyright 2010
Definition
Benign prostatic hypertreophy or BPH is a hyperplastic process of the prostate and is therefore a misnomer . The cause is uncertain, but requires androgens to occur. Estrogens, neurotransmitters, growth factors, and stromal-epithelial interactions may also play a role in modulating this process. While normal cells undergo a programmed cell death, in the setting of BPH, this process is blocked.
Structurally the disorder is characterized by a proliferation of the epithelial and stromal cells in the periurethral area of the prostate.
Functionally, this disorder may contribute to neurogenic changes in the bladder contractility. As a result of proliferation and hypertropy, pressure exerted on the urethra obstructs bladder outflow. The increased filling of the bladder results in urgency. Since greater pressure is required to overcome the obstruction, incomplete voiding of the bladder is common. This elevated post-void residual leaves the bladder little additional capacity for urine produced, resulting in frequency and nocturia. As the bladder overflows, dribbling may also result.
Clinically, this process contributes to the majority of lower urinary tract symptoms in men. The long term clinical consequences of BPH are uncertain, as the natural history is poorly understood.
Imaging is not routinely performed for the evaluation of BPH, however ultrasound, MRI are useful. Determination of prostatic size may also be estimated using digital rectal examination (DRE) As it is technically a histologic diagnosis, confirmation usually requires examination of tissue from biopsy, surgery or autopsy. The greatest impact of BPH is on quality of life, related to urinary symptoms, and thus severity is most usefully measured using the American Urological Association Symptom Index (AUASI), developed in 1992. This is a questionnaire of 7 questions pertaining to urinary symptoms, i.e. frequency, urgency, hesitancy. Alternatively, urinary flow rates, and measurements of Prostate Specific Antigen may be used as adjuncts.
Treatment may span from pharmacologic, such as androgen deprivation therapy, minimally invasive surgical therapy, and transurethral resection of the prostate (TURP).
Zonal Anatomy and Predilections For Disease
The prostate gland can be viewed as having 4 major zones. The outer zone is called the peripheral zone, accounts for 70% of the parenchyma. Inward of the peripheral zone is the central zone that accounts for 25% of the parenchyma. The periurethral zone is called the transitional zone and fibromuscular zone (anterior layer) account for the remaining 5% of parenchyma.
|
Zonal Anatomy and Predilections For Disease |
|
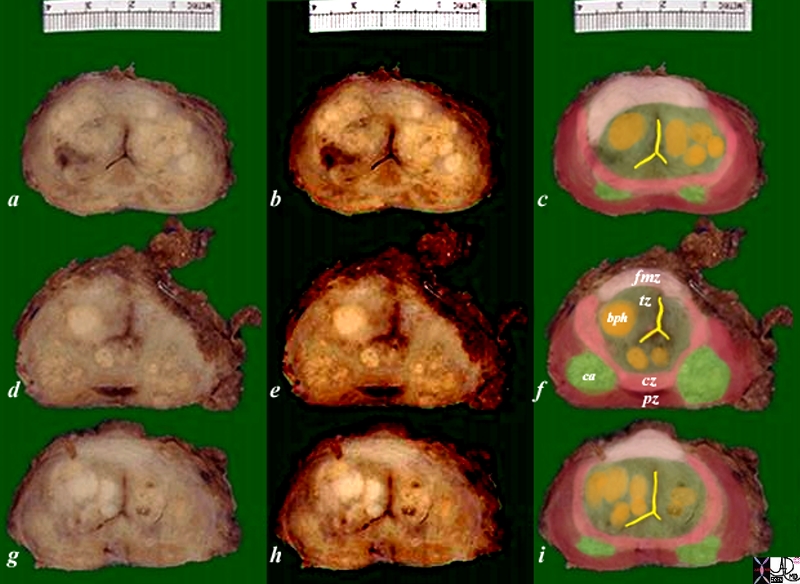
The diagram depicts the zonal morphology relevant to the locations where disease arises. The normal gland is seen in image (a). The prostate gland can be viewed as having 4 major zones. The outer zone is called the peripheral zone, accounts for 70% of the parenchyma. Inward of the peripheral zone is the central zone that accounts for 25% of the parenchyma. The periurethral zone is called the transitional zone and fibromuscular zone (anterior layer) account for the remaining 5% of parenchyma. Image (b) shows BPH (benign prostatic hypertrophy) which is caused by hyperplasia and enlargement of the transitional zone. Image (c) shows carcinoma (bright lime green) arising from the peripheral zone which is the characteristic site of origin of this disease. Image (d) shows a combination of BPH in the transitional zone and carcinoma in the peripheral zone. This is a common combination of diseases in the elderly population. Image Courtesy Ashley Davidoff MD Copyright 2010 25078cL01.8s |
|
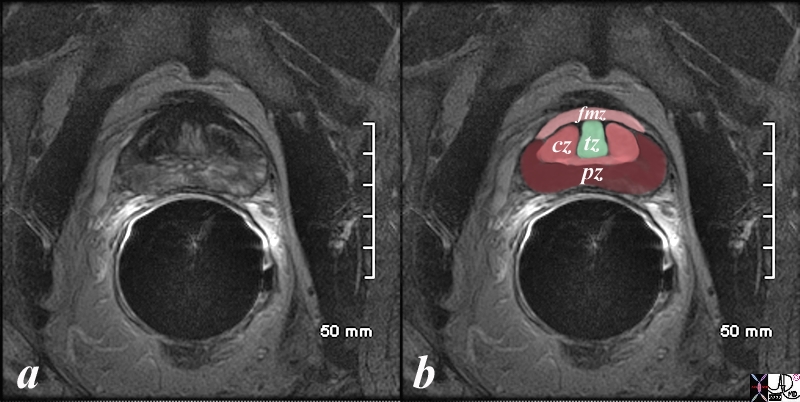
Normal Zonal Anatomy MRI T2 Weighted |
|
The patient is a 60 year old man. His MRI was performed with a transrectal coil and the image shows the T2 weighted sequence in the axial projection (a,b). The scan shown demonstrates the normal zonal anatomy of the prostate. The prostate gland can be viewed as having 4 major zones. In the normal gland the outer zone called the peripheral zone, accounts for 70% of the parenchyma. (maroon, pz). It is often canoe shaped in the axial projection. Inward of the peripheral zone is the central zone (dark pink, cz) that accounts for 25% of the parenchyma. The remaining 5% of the parenchyma is composed of the periurethral zone called the transitional zone (light green), and the fibromuscular zone (light pink, fmz) – the anterior most layer. Image Courtesy Ashley Davidoff MD Copyright 2010 98877c.8s |
|
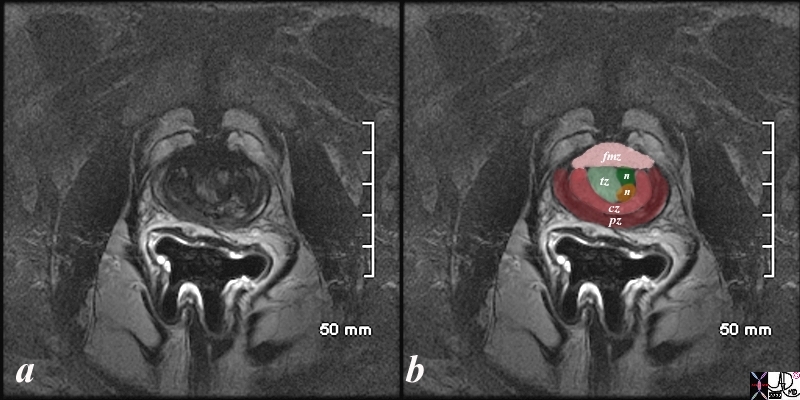
Early Expansion of the Transitional Zone with Two Nodules BPH |
|
The patient is a 61 year old man. His MRI was performed with a transrectal coil and the image shows the T2 weighted sequence in the axial projection (a,b). The scan shown demonstrates the normal zonal anatomy of the prostate but shows early enlargement of the transitional zone with two nodules participating in the expansion (n in b). The prostate gland can be viewed as having 4 major zones. In the normal gland the outer zone called the peripheral zone, accounts for 70% of the parenchyma. (maroon, pz). It is often canoe shaped in the axial projection. Inward of the peripheral zone is the central zone (dark pink, cz) that accounts for 25% of the parenchyma. The remaining 5% of the parenchyma is composed of the periurethral zone called the transitional zone (light green), and the fibromuscular zone (light pink, fmz) – the anterior most layer. Image Courtesy Ashley Davidoff MD Copyright 2010 99052c.8s |

BPH – Benign Prostatic Hypertrophy |
|
The 70 year old male shows an enlarged prostate with two distinct zones measuring 7.2cms in A-P by 6.1cms. The posterior layer seen in b overlaid in maroon as labeled pz = peripheral zone is recognized by its shape and location. In ward of this layer a combination of zones that exist in the isodense layer. Since the prostate gland has 4 major zones and we have accounted for the peripheral zone (pz) 3 other layers exist . Inward of the peripheral zone is the central zone followed by the transitional zone and finally the anterior fibromuscular layer In this patient who has benign prostatic hypertrophy (BPH) the transitional zone is enlarged due to hyperplasia and hypothetically illustrated in c. Note that BPH is a misnomer because the enlargement is due to hyperplasia and not hypertrophy. Image Courtesy Ashley Davidoff MD Copyright 2010 25078c04bL01.8s |
|
Carcinoma and BPH |
|
The pathology specimen is from a patient with prostate carcinoma and benign prostatic hyperplasia. Image Courtesy Alexander Perepletchikov MD PhD 99379c03L.8s |

BPH Homogeneous Gland |
|
The CTscan is from a patient with an enlarged prostate. The anterior aspect of the gland protrudes with two symmetrical homogeneous components likely representing an enlarged transitional zone and prostate hyperplasia though by the nature of the disease the combination of cancer and BPH commonly coexist. The urinary bladder wall is minimally thickened. Image Courtesy Ashley Davidoff MD Copyright 2010 25517b.8s |

Acute Retention and Renal Obstruction |
|
The CT scans show an enlarged prostate (a) with an enlarged bladder (b) hydroureter (c, yellow arrow) and extravasated urine (orange arrow c and d) with hydronephrosis These findings are consistent with acute obstruction of the kidneys and bladder as a result of prostatic enlargement. Image Courtesy Ashley Davidoff MD Copyright 2010 17069c.8s |
Surgical Treatment of BPH
There are 3 main surgical options for treatment of BPH: 1) transurethral resection of the prostate (TURP), 2) transurethral incision of the prostate (TUIP), and 3) open prostatectomy.
TURP:
This is the gold standard for effective treatment for BPH. The procedure is performed using a scope designed to pass through the urethra and allow a wire loop with electrical current to remove chips of prostatic tissue. Patients usually require an overnight stay in the hospital. Major complications of this procedure are bleeding, hyponatremia from absorption of free water, incontinence, and retrograde ejaculation. Operative time is generally limited to 1 hour in order to prevent this hyponatremia.
TUIP
TUIP is similar to TURP. However, instead of removing prostatic tissue, an electrical knife is used to make small cuts in the prostate.
Open Prostatectomy
Open prostatectomy can be performed for extremely large prostates either through a suprapubic or perineal approach. This is a more invasive procedure with higher complications include bleeding and infection.
Other
Other minimally invasive procedures include: 1) laser prostatectomy, 2) transurethral microwave thermotherapy (TUMT), high intensitry focused ultrasound (HIFU), transurethral needle ablation (TUNA), prostatic stents, and transurethral electrovaporization.
Laser Prostatectomy:
This technique utilizes a laser with various wavelengths. There is a decreased risk of bleeding, fluid absorption, retrograde ejaculation, impotence, and incontinence. Patients usually require a shorter hospitalization and sometimes can be done as an outpatient. performed with the use of a laser with various types and wavelengths have the advantages of lack or decreased risk of complications such as intraoperative bleeding and fluid absorption, retrograde ejaculation, impotence, and incontinence. Patients undergoing this procedure tend to require shorter hospital stays and can be admitted on an outpatient basis.
TUMT:
This technique uses microwave energy with frequencies between 915-2450 MHz to heat tissues. This procedure can be done as an outpatient with local anesthesia. It is safer than a TURP but not as effective.
HIFU:
HIFU uses ultrasonic energy to heat the prostate. This is done transrectally.
TUNA:
TUNA uses high-frequency radio wave to cause thermal injury to the prostate. Needles are inserted into the prostate and energy is delivered through them to localized areas. The procedure only requires local anesthesia.
Prostatic stents:
These are permanent, flexible, expanding devices placed in the urethra to expand the lumen. Advantages of this procedure include: short operative time, minimal bleeding, no need for post-operative catheter, and no need for a hospital stay.
Transurethral electovaporization:
This technique simultaneously vaporizes and coagulated prostatic tissue so no bleeding or fluid absorption occurs. Operative times can be much longer than an hour, therefore much larger glands can be operated on.