The Common vein Copyright 2010
Introduction
MRI of the prostate gland at present is being used only in the evaluation of primary prostate cancer. In this context, MRI provides improved tissue contrast and anatomic detail compared with ultrasound and CT.
Principles
The appearance of the prostate gland on T1 and T2-weighted sequences has histologic correlates to the gland’s zonal anatomy. The central gland, comprised of the central and the transition zones of the prostate, is an arrangement of compact smooth muscle and loose glandular tissue. In contrast, the peripheral gland is predominantly made up of mucin-rich glandular tissue. On T1- weighted sequences, the entire gland demonstrates uniform intermediate signal, leaving the zonal anatomy indistinguishable. On T2 however, the central gland demonstrates low to intermediate signal intensity while the normal peripheral gland is hyperintense. Thin collagenous septa within the peripheral gland appear hypointense on T2. The prostatic capsule, which surrounds the entire gland, as well as the surgical capsule, which separates the central and peripheral glands, also appear hypointense on T2. T2-weighted sequences thus represent the necessary diagnostic images for evaluation of prostate gland on MRI.
The role of MRI in guiding prostatic interventions has also been under investigation. MRI-guided percutaneous needle biopsy of the prostate may be considered when prostate cancer is suspected in patients with rising PSA and a negative transrectal ultrasound-guided (TRUS) biopsy or a proctocolectomy. In these settings, MRI may demonstrate the tumor and guide needle placement for accurate diagnostic sampling. Similarly, MRI-guided brachytherapy seed placement in the prostate gland can also be performed in patients with prior proctocolectomy as they are not candidates for US-guided treatment.
Historical Aspects
Initial reports of MRI localization and staging of prostate cancer date back to the 1980s. At that time decreased spatial and contrast resolution, low signal to noise ratio, low magnetic strength (0.3 tesla) and lack of utilization of endorectal coils resulted in suboptimal imaging. Overall examination time was too long. The emphasis at that time was placed on deriving optimal sequences for the evaluation of the prostate gland and the pelvis.
Current MRI technology utilizes 1.5 T along with a phased-array pelvic coil and an endorectal coil. Images demonstrate better anatomic detail and they are obtained in a shorter time frame. Use of 3.0 T scanner is also being investigated for imaging of the prostate gland.
Functional imaging of the prostate, as a means to overcome the shortcomings of the anatomic evaluation, is gaining popularity. Functional imaging involves techniques including spectroscopy, diffusion weighted imaging (DWI), dynamic contrast enhancement with gadolinium, and the use of superparamagnetic nanoparticles (an iron-based contrast agent). The latter is currently limited to the research arena and is being evaluated for use in detection of nodal metastases from prostate cancer.
MRI spectroscopy leverages the altered levels of choline and citrate in prostate cancer tissue. Citrate level, normally high in the prostate gland, is decreased in prostate cancer. Choline metabolism, on the other hand, is increased in cancerous tissue. Together, the changes result in an overall increase in choline to citrate ratio which is demonstrated by spectroscopy.
DWI in detection of prostate cancer is similar in principle to stroke imaging of the brain. Cancerous tissue has more restricted movement of water molecules than does normal tissue. This restriction results in an increased signal on DWI sequence in prostrate cancer along with a corresponding low signal on ADC map.
Contrast enhancement of prostate cancer after injection of gadolinium also operates on the principle noted with tumors in other parts of the body. After obtaining dynamic contrast enhanced images, perfusion parameters are measured to detect and differentiate cancer from normal prostate tissue.
Indications
Prostate MRI is currently performed for local and distant staging in patients with biopsy-proven prostate cancer. It is also used for localizing and detecting cancer in patients with rising PSA levels and negative TRUS-guided biopsies.
Contraindications
Same as those for MRI of any other organ. No specific contraindications for prostate MRI.
Advantages
MRI is a noninvasive method of evaluation for prostate cancer, for which the convention otherwise is TRUS-guided biopsies. Neither ultrasound nor CT provides anatomic detail afforded by MRI.
Disadvantages
Endorectal coil can be uncomfortable for patients during placement and for the duration of the examination. The MRI appearance of cancer and benign entities in the peripheral zone may be similar, and this limits its utility in diagnosis. MRI appearance of cancer may also look similar to the normal tissue of the central and transitional zones of the prostate gland.
Aim
The purpose of this exam is to evaluate extension of known prostate cancer outside of the prostatic capsule, including the neurovascular bundles, seminal vesicles and other pelvic organs as well as the surrounding lymph nodes and osseous structures to help in guiding management.
Method
Patient preparation
Prostate MRI is deferred for 6-8 weeks after prostate biopsy to avoid interference of post-biopsy hemorrhage in detecting tumor within the gland. Patients are asked to eat a light meal and to avoid caffeine for 4 hours prior to the examination. Patients are also asked to administer a fleet enema in the morning of the exam or 2 hours prior to the exam for placement of an endorectal coil before the MRI. For placement of the coil, the patient is placed in the fetal position on the scanner table and then turned into supine position for the duration of the exam.
Equipment
Prostate MRI requires the use of endorectal coil (a receiver-only coil) in addition to pelvic phased-array coil. The scanner usually employed is 1.5 T.
Technique
Anatomic MRI of the prostate generally utilizes non-contrast enhanced fast spin-echo T1-weighted and T2-weighted sequences. A typical protocol involves triplanar (axial, sagittal, and coronal planes) T2-weighted images through the prostate gland with thin 3-4 mm sections and small 14-20 cm field-of-view (FOV); axial T1-weighted images through the prostate gland with small FOV; and axial T1-weighted images through the pelvis with wide FOV for evaluation of nodal and osseous metastases. The latter may be extended into the retroperitoneum for evaluation of distant lymphadenopathy.
|
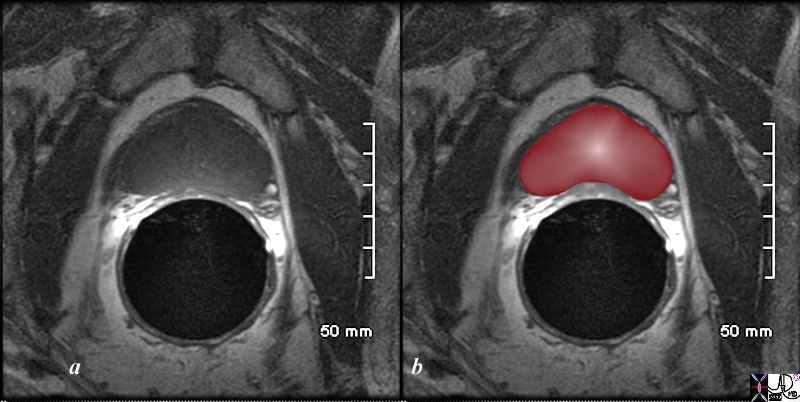
Heart Shaped Structure in the Transverse Dimension T1 Weighted Transrectal MRI |
|
The patient is a 60 year old man. His MRI was performed with a transrectal coil and the image shows the T1 weighted sequence in the axial projection (a,b). The scan shown demonstrates the normal heart shape of the prostate at this level in the axial projection. Zonal anatomy cannot be distinguished since the T1 weighted sequence results in a homogenous signal from all the zones. Image Courtesy Ashley Davidoff MD Copyright 2010 98874cL.8s |
DWI and gadolinium enhanced sequences may also be added with the potential to improve detection of prostate cancer. Dynamic 3D fat suppressed images in the axial plane after injection of gadolinium are also obtained in many centers.
Result
Cancer in peripheral zone appears hypointense on T2-weighted images. While hemorrhage also appears hypointense on T2, it may be differentiated from cancer on T1-weighted sequences on which hemorrhage appears hyperintense. Inflammation, infection, post-treatment fibrosis, and other post treatment-related changes also appear hypointense on T2 which may reduce specificity of cancer detection.
Extension of prostate cancer outside of the prostatic capsule may be diagnosed on T2 when hypointense signal is seen extending outside of the capsule. The signal may also be noted to involve the neurovascular bundle. It may be seen as a focal bulge in peripheral zone of the gland. Short, linear, low signal hypointensities may be seen extending from the peripheral zone into the periprostatic fat.
Prostate cancer at the base of the gland may extend superiorly to involve the seminal vesicles. In this instance, hypointense signal within the normally T2 hyperintense seminal vesicles is indicative of metastatic disease to seminal vesicles.
The central gland should be closely evaluated for tumor in patients with negative biopsies in the context of rising PSA level. With malignant involvement, the usually heterogeneously hypointense central gland on T2 may demonstrate a focal area of slightly decreased signal. Combination of T2-weighted anatomic sequences with functional imaging, specifically spectroscopy, has demonstrated improved tumor detection in central gland.
There is a wide range of sensitivity and specificity, 77%-91% and 27%-61% respectively, for detection of prostate cancer with T2-weighted MRI performed with endorectal coil. While these numbers are generally improved with the addition of either of the previously mentioned functional imaging methods, there still exists significant variation in sensitivity and specificity among studies.
|
Zonal Anatomy and Predilections For Carcinoma – Peripheral Zone |
|
The diagram depicts the zonal morphology relevant to the locations where disease arises. The normal gland is seen in image (a). The prostate gland can be viewed as having 4 major zones. The outer zone is called the peripheral zone, accounts for 70% of the parenchyma. Inward of the peripheral zone is the central zone that accounts for 25% of the parenchyma. The periurethral zone is called the transitional zone and fibromuscular zone (anterior layer) account for the remaining 5% of parenchyma. Image (b) shows BPH (benign prostatic hypertrophy) which is caused by hyperplasia and enlargement of the transitional zone. Image (c) shows carcinoma (bright lime green) arising from the peripheral zone which is the characteristic site of origin of this disease. Image (d) shows a combination of BPH in the transitional zone and carcinoma in the peripheral zone. This is a common combination of diseases in the elderly population. Image Courtesy Ashley Davidoff MD Copyright 2010 25078cL01.8s |
|
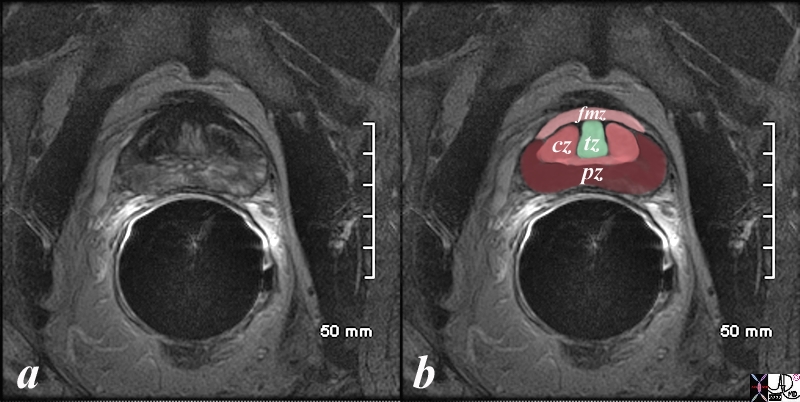
Normal Zonal Anatomy MRI T2 Weighted |
|
The patient is a 60 year old man. His MRI was performed with a transrectal coil and the image shows the T2 weighted sequence in the axial projection (a,b). The scan shown demonstrates the normal zonal anatomy of the prostate. The prostate gland can be viewed as having 4 major zones. In the normal gland the outer zone called the peripheral zone, accounts for 70% of the parenchyma. (maroon, pz). It is often canoe shaped in the axial projection. Inward of the peripheral zone is the central zone (dark pink, cz) that accounts for 25% of the parenchyma. The remaining 5% of the parenchyma is composed of the periurethral zone called the transitional zone (light green), and the fibromuscular zone (light pink, fmz) – the anterior most layer. Image Courtesy Ashley Davidoff MD Copyright 2010 98877c.8s |
|
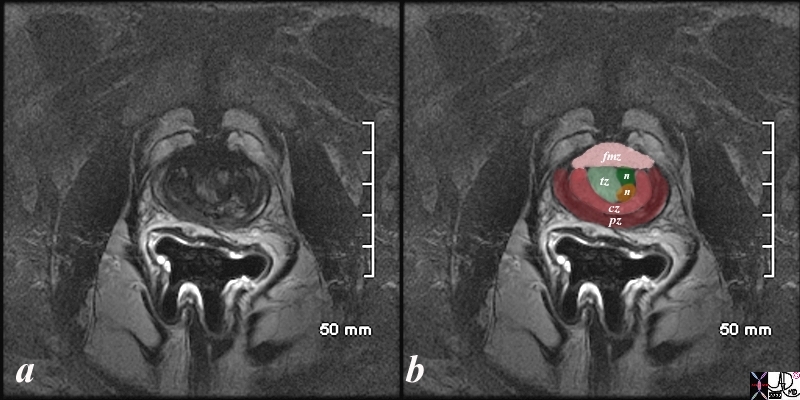
Early Expansion of the Transitional Zone with Two Nodules BPH |
|
The patient is a 61 year old man. His MRI was performed with a transrectal coil and the image shows the T2 weighted sequence in the axial projection (a,b). The scan shown demonstrates the normal zonal anatomy of the prostate but shows early enlargement of the transitional zone with two nodules participating in the expansion (n in b). The prostate gland can be viewed as having 4 major zones. In the normal gland the outer zone called the peripheral zone, accounts for 70% of the parenchyma. (maroon, pz). It is often canoe shaped in the axial projection. Inward of the peripheral zone is the central zone (dark pink, cz) that accounts for 25% of the parenchyma. The remaining 5% of the parenchyma is composed of the periurethral zone called the transitional zone (light green), and the fibromuscular zone (light pink, fmz) – the anterior most layer. Image Courtesy Ashley Davidoff MD Copyright 2010 99052c.8s |
|
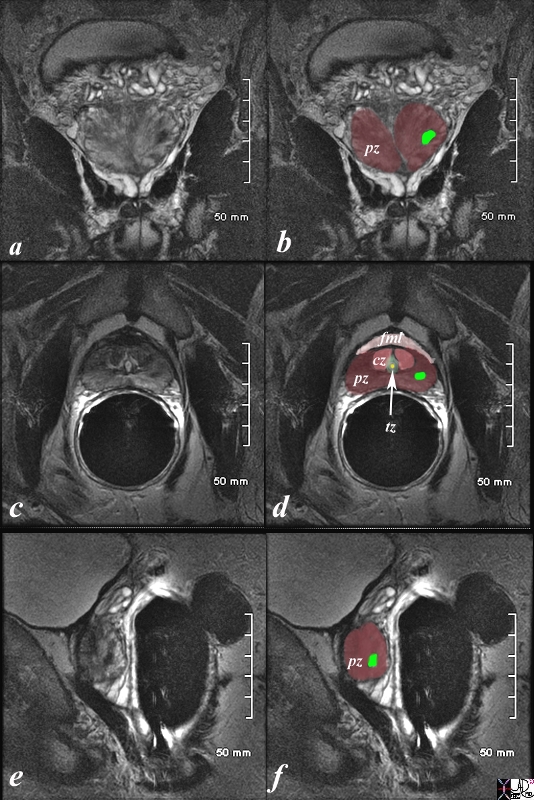
Prostate Carcinoma MRI T2 Weighted |
|
The patient is a 61 year old man with primary prostate carcinoma. His MRI was performed with a transrectal coil. T2 weighted images in the coronal projection (a,b), axial projection (c,d), and sagittal projection (e,f) are shown. The primary lesion is a 8mm lesion ( bright green overlay in b,d,f) is hypointense on the T2 weighted image and noted in left sided peripheral zone (pz darker maroon b,d,f). Other zones noted include central zone (lighter red, cz, in d) transitional zone (pale green,white arrow, tz, in d) and fibromuscular layer (light pink, fbl in d). The urethra is shown in yellow in the middle of the tz in d. The lesion was biopsied and shown to be an adenocarcinoma of the prostate. Image Courtesy Ashley Davidoff MD Copyright 2010 98899cL02.8s |
|
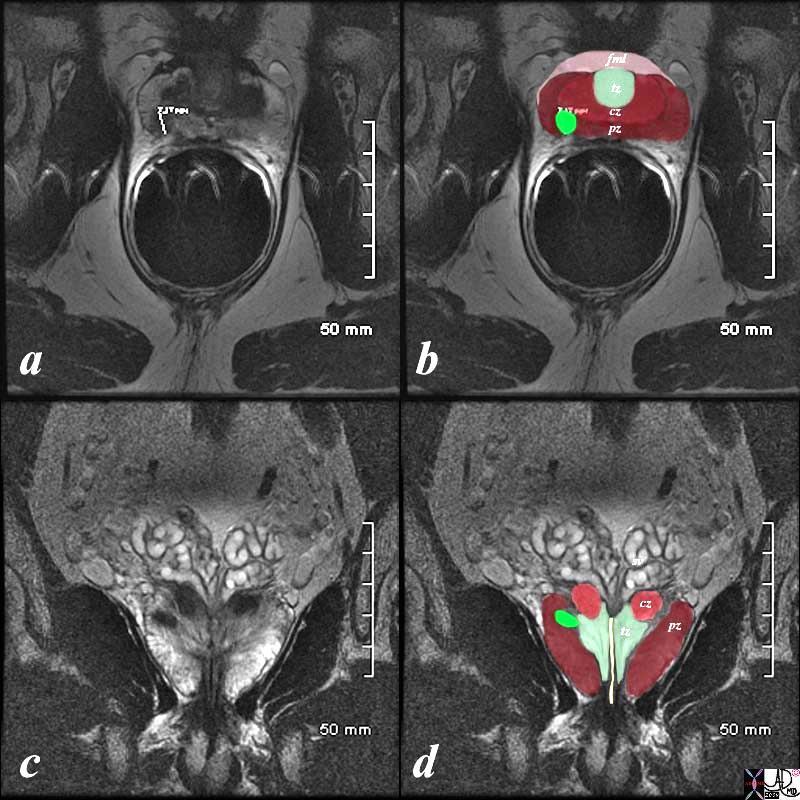
Right Peripheral Zone MRI T2 Weighted – Endorectal Coil |
|
The patient is a 60 year old man with primary prostate carcinoma. His MRI was performed with a transrectal coil and T2 weighted images in the axial projection (a,b) and coronal projection are shown. The primary lesion is a 8mm lesion ( bright green overlay in b and d) is hypointense on the T2 weighted image (a, b) and noted in the right sided of the peripheral zone (pz darker maroon). Other zones noted include central zone (lighter maroon, cz, in b,d) transitional zone (pale green, tz, in b,d) and fibromuscular layer (light pink, fbm in b) The lesion was biopsied and shown to be an adenocarcinoma of the prostate. Image Courtesy Ashley Davidoff MD Copyright 2010 99320cL.8s |
Potential Complications
Endorectal coil placement may result in rectal erosion, bleeding and proctitis. These complications are more pronounced if endorectal coil placement is done soon after a transrectal prostate biopsy.
Allergic reaction to gadolinium and nephrogenic systemic fibrosis in patients with renal failure may occur with MRI of any organ performed with contrast injection.
Conclusion
MRI of prostate gland is an evolving technique for noninvasive evaluation for prostate cancer. At present, T2-weighted sequence is the workhorse of prostate MRI as it best depicts prostate anatomy and extension of tumor outside of the gland. Functional imaging of the prostate holds promise in improving detection of prostate cancer.